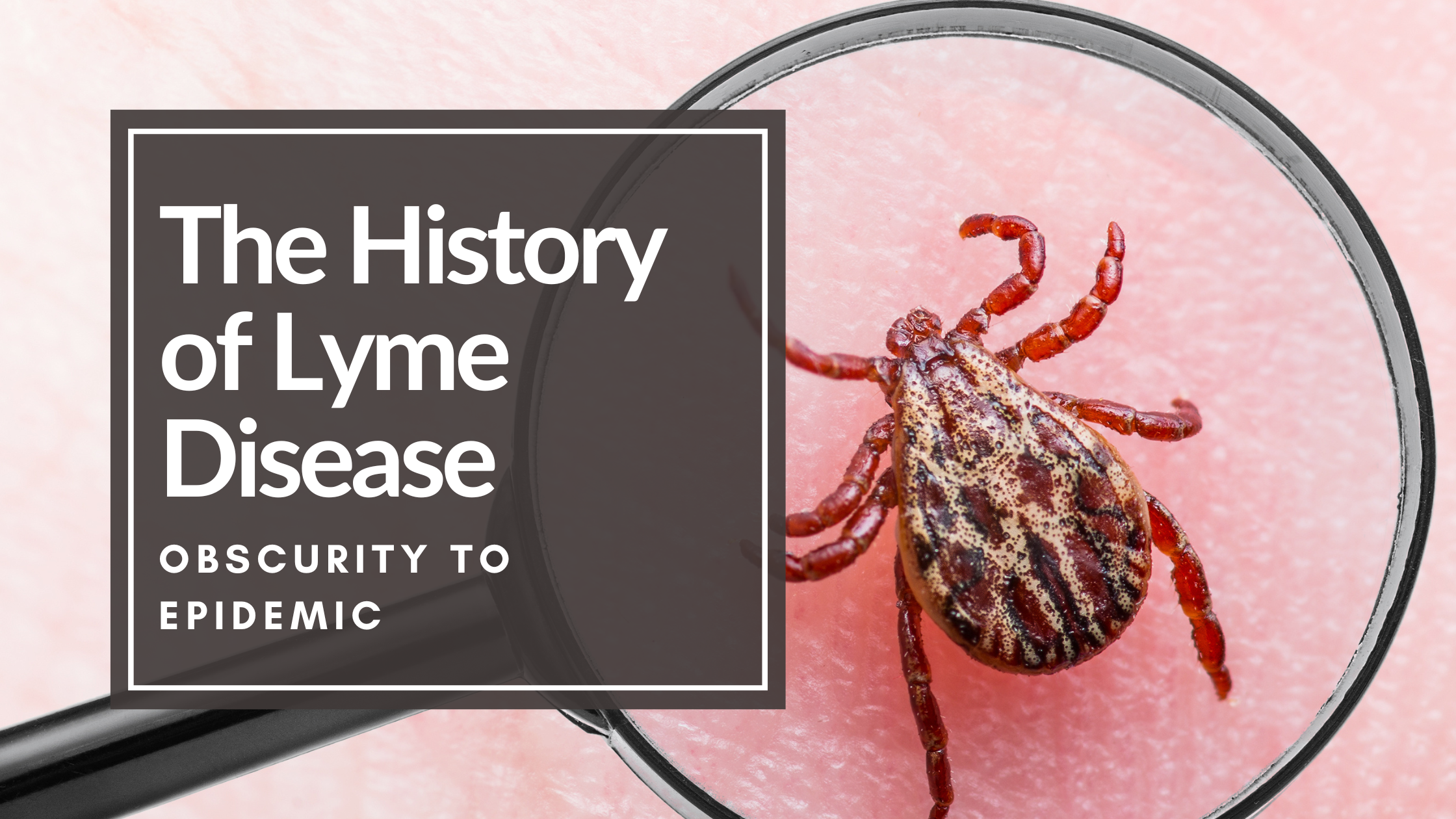
What is the History of Lyme Disease?
The history of Lyme Disease has a long standing past, even as you see this tick-borne illness become a growing epidemic in the United States and around the world. Although it was only identified as a specific disease in the 1970s, it is believed to have been around for centuries.
This article provides a comprehensive look at the history of Lyme disease, including its origins, early recognition, diagnosis, treatment, and prevention.
History of Lyme Disease: An Introduction
Lyme disease is caused by a bacterium called Borrelia burgdorferi. It is transmitted to humans through the bite of infected ticks and other biting insects like mosquitos, fleas, and mites. The symptoms of immediate or acute infection with the bacteria can vary widely and can include fever, headache, pain, fatigue, and a characteristic (maybe) skin rash.
If left untreated, Lyme disease can lead to more serious health problems such as arthritis, heart problems, and nervous system disorders.
The History of Lyme Disease
Lyme disease is believed to have originated in the northeastern United States, particularly in the rural areas of Connecticut. The first cluster of unique cases of arthritis-like symptoms, which was later called Lyme disease, occurred in 1975 in the town of Old Lyme, Connecticut. A mother let the state health department know of a cluster of children from their small community had a common diagnosis of juvenile arthritis. Some had a ringlike rash before the joint pain started.
However, there is evidence that Lyme disease has been around for centuries. In fact, there are records of a disease with similar symptoms to Lyme disease dating back to the 1700s.
Alan Barbour MD writes that in 1909, the monthly meeting of the Dermatological Society gathered to discuss a case of erythema migrans in an older woman, and the patient’s doctor thought that this red bullseye rash came from an Ixodes Reduvius tick (1).
In 1704, Dr. John Walker may have described one of the first accounts of Lyme in people with limb pain on an island off the coast of Scotland (2).
In 1991, the corpse of the Iceman, or Ötzi, was found in the Tyrolean Alps, and research later discovered that the corpse contained almost two-thirds of the genome of Borrelia, the bacteria genus of bacteria linked to Lyme Disease (3).
Whether this bacteria is new or old, it can travel and wreak havoc on almost any body system.
History of Lyme Disease: The Discovery of the Bacteria
In 1982, Willy Burgdorfer, a scientist working for the National Institutes of Health, took a tick and looked at its gut contents under a microscope. He saw a “thread-like bacteria” that he recognized as the species Borrelia, which belongs to the bacterial family that causes relapsing fever (4). Testing in lab animals revealed the same symptoms as the children in question in Old Lyme, Connecticut, and further investigation revealed the same bacterial spirochete in both the tested animals and those with Lyme.
The bacteria was named Borrelia burgdorferi in his honor. Some say this discovery allowed for more accurate diagnosis and treatment of Lyme disease.
A spirochete bacteria is like a corkscrew, and they look like a worm under a microscope. There are many different species of spirochetes, and not all of them make us sick however many of them can. A Borrelia infection is properly termed borreliosis (5). Some cause something called a relapsing fever borreliosis, and some cause non-relapsing. If you think that this is confusing, you would be right.
There are many bacteria that cause the symptoms of borreliosis, or Lyme disease, and they are generally called co-infections.
If you want to learn the basics of Lyme Co-infections, go to this blog post:
When discussing the history of Lyme disease, the terminology of Lyme has also undergone so much change and controversy.
For example, many of our affiliate practitioners use the term: “Lyme co-infections.” The proper term for Lyme co-infections, according to author and master herbalist Stephen Harrod Buhner, is arthropod-transmitted infections group, or ATIG. This refers to the evidence that these bacteria do not only come with ticks but arthropods, which can be spiders and other insects.
We use the term obscure in the title of this blog post to allude to the uncertainty and controversy over this group of bacteria, transmission, and the disease itself.
History of Lyme Disease: Symptoms
The symptoms of Lyme disease can vary widely, just like the organisms causing the symptoms can vary. When a tick latches on to you or your dog, it starts to dine on your blood supply, and the blood goes into the tick’s stomach. This is where the microorganisms live. The tick will, at some point, release the contents of the stomach back into the individual person or pet.
There is controversy over the timeline of this action, from minutes to days. As Dr. Neil Nathan says in his book Toxic, “The tick, however, does not have a wristwatch and sometimes will release its contents much sooner, so there is no time frame that is truly safe.”
The symptoms of Borrelia, or Lyme, according to the CDC, include:
- fever
- rash
- headache
- fatigue
The CDC also notes tick-borne illness symptoms as being the same and include joint pain and muscle aches on the list.
History of Lyme Disease: A Tough Diagnosis
The most common diagnostic tests for Lyme disease are:
- a blood test, the ELISA test, which detects antibodies to the bacterium that causes the disease. ELISA stands for enzyme-linked immunoassay.
- the Western Blot test.
Both assess antigens in a blood sample and/or the presence of the bacteria itself.
There are questions behind the sensitivity of the tests due to the multiple species of Borrelia bacteria that may not be targeted for detection with certain tests. Timing is important in these tests, as a person needs time to make the antibodies to be detected in the ELISA test.
This is one reason why many have turned to other testing methods, including bioenergetics with CBH Energetics, for a different look at their body and symptoms.
It is important to remember that bioenergetics is not diagnostic in nature, but it does identify areas of energetic stress in the body and energetic toxins.
History of Lyme Disease: Constant Controversy
There is a controversial debate in the medical community about chronic Lyme disease. Some doctors believe that Lyme disease can persist in the body even after treatment and can lead to chronic symptoms such as fatigue and joint pain. However, other doctors believe that these symptoms are not caused by Lyme disease and are instead the result of other factors such as stress or anxiety.
This may be due to the unique nature of the Borrelia species in general. When they enter a new environment, they can shift their genomic structure to fit their host. This may be one reason why symptoms persist (5).
They are thin and tiny and can elude magnification. They have a tail called flagella that propels them through their environment. They move. Their movement is enhanced by a unique flagella system that is through their body, and they are protected by an outer protein coat (5).
These spirochetes are said to be really fast. They can evade parts of the immune system, like white blood cells, and they can alter themselves. They can “encyst” or enclose themselves as a protection mechanism.
They also seem to find protected places to hide, including in biofilm. Biofilms are colonies of microbes that secrete substances to make them stick together and evade the body’s defense systems. Borrelia species can become part of the human or pet biofilm.
Lyme Disease Treatment and Prevention
The treatment of Lyme disease within the modern medical community typically involves a course of antibiotics. The length of treatment depends on the stage of the disease and the severity of the symptoms.
There is controversy over the effectiveness of this approach in the long term, as there seems to be persistence, broadening, or worsening of symptoms long after treatment is over. This brings up the topic of the stages of Lyme disease, which needs its own blog post!
Today, we will focus on prevention, as this is one of the best ways to elude Lyme disease in the first place! Prevention of tick bites includes:
- Dress appropriately! Wear long sleeved shirts, and long pants, tuck your shirt into your pants, and your pants into your socks. Do not wear open-toed shoes.
- Use some sort of repellant. Many common sites recommend DEET, which also contributes to overall toxicity. Explore options like lemon eucalyptus oil, cedar oil, peppermint, apple cider vinegar, neem, and thyme oil. Choose some and make a mixture.
- Shower after a walk in the woods, and shower your dog too!
- Garlic oil is another option for trick prevention.
Ultimately, you know your area, and choosing to use a commercial bug spray is yours. Just be aware that there are cons to using insecticides for you and the environment.
The Global Impact of Lyme Disease
Some websites list the top places where Lyme disease is found in the U.S., but make no mistake: Lyme and Borrelia bacteria, among the others that cause the same symptoms, are not just a problem in the United States.
This is a growing problem in other parts of the world, including Europe and Asia. In fact, it is estimated that there are over 300,000 cases of Lyme disease in the United States each year and over 65,000 cases in Europe.
History of Lyme Disease: Awareness is Growing
Lyme disease is a serious illness that can have long-term health consequences if left untreated and undiagnosed.
There are many comprehensive resources for clients, including:
Be aware of the symptoms of Lyme disease and co-infections, and take steps to prevent tick bites. At CBH Energetics, we have our Living With Lyme fund and contest that runs year-round!
We highlight Living With Lyme in May, during Lyme Awareness Month, however this is open year round!
CBH Energetics gives away approximately $2500 in testing, remedies, and consultations to one person every year. This contest was inspired by owner and founder Samantha Stupak.
Read Samantha’s own Lyme disease journey here and understand the impact of bioenergetic testing.
Sources:
- Lyme Disease, by Alan Barbour MD
- Recovery from Lyme Disease
- https://www.nature.com/articles/nature.2012.10130.pdf
- Bitten, Kris Newby
- Healing Lyme, by Stephen Harrod Buhner
- Toxic: Heal Your Body From Mold Toxicity, Lyme Disease, Multiple Chemical Sensitivities, and Chronic Environmental Illness, by Neil Nathan MD
DISCLAIMER: Balanced Health, LLC/CBH Energetics and any parent, subsidiary, affiliated or related entities and companies do not provide medical advice or services. This post is for educational and informational purposes only and is not intended to diagnose, treat, cure, or prevent any disease, condition, complaint, illness or medical condition and are not a substitute for professional services or medical advice. Seek the advice of a physician or other qualified healthcare professional with any questions you may have. Never disregard professional medical advice or delay seeking treatment.